Antibiotic resistant genes lurk in city parks
Overuse of antibiotics has led to superbugs that resist even powerful last-line-of-defense antibiotics. UCLA researchers have learned that antibiotic resistant genes are everywhere, including places people are encouraged to go for fun—parks.
Antibiotic-resistant superbugs have health experts on high alert, and for good reason.
They currently kill 23,000 people each year in the United States, and with antibiotic resistance rapidly increasing, worldwide they are expected to kill 10 million annually by 2050—more than cancer.
The anxiety over superbugs is likely to grow in California, where UCLA researchers recently discovered high levels of antibiotic-resistant genes (ARGs)—which lead to drug-resistant bacteria—in the parks of four cities.
Concentrations varied, but in general, air, soil and water from city parks in Los Angeles, San Diego, Fresno and Bakersfield contained high quantities of the genes, according to a study published today.
The highest levels in tap water came from drinking fountains in San Diego and Los Angeles, catching researchers by surprise. A previous study had uncovered high levels in air near concentrated animal feeding operations, so the biggest numbers were expected to come from Bakersfield and Fresno.
Jennifer Jay, a professor of environmental engineering at UCLA and one of the paper’s authors, stressed that although the findings are significant, it’s not time to panic.
“We don’t want to sound alarm bells and have people afraid that they’d be breathing ARGs while they’re in the shower,” Jay said.
That’s because ARGs are not directly toxic, especially when they’re just floating around on benign bacteria cells. The trouble comes when these genes become part of pathogenic organisms—the ones that make us sick. Resistant genes get transferred to pathogens when cells reproduce, get infected by viruses or through uptake of free-floating DNA.
Ever since life started on Earth about 3.5 billion years ago, bacteria have produced antibiotics to kill off competitors. In response, antibiotic resistant genes became a first line of defense in a microbial survival race. In recent years, overreliance on antibiotic drugs by medical and livestock industries caused these genes to proliferate exponentially.
One worrisome characteristic is ARGs’ ability to persist in the environment. Many contaminants degrade over time or, at worst, stick around at consistent levels. “One mercury ion can’t spontaneously become two mercury ions,” said Cristina Echeverria-Palencia, the study’s lead author and an environmental engineering researcher in Jay’s lab. “However, once genes get inside a bacteria cell, every time that cell replicates, so does the gene.”
ARGs are currently considered an “emerging contaminant”—even though they’re on the rise, there isn’t enough data to know how many more are present than would occur naturally.
In all 24 parks surveyed across the four cities, soil contained high levels of a gene that resists the antibiotic Sulphadimidine.
“Sulphadimidine was the first mass-manufactured antibiotic. We no longer use it because basically we over-used it,” said Echeverria-Palencia. “But [the resistant gene] has the ability to remain in the environment for a long time and has been linked to hyper-resistance.”
UCLA’s Cody Ericksen contributed to the study through the senior practicum, a yearlong program in which undergraduate students devise science-based solutions to real-world environmental problems. “There are always unforeseen problems with getting samples,” Erikson said. In this case, to prevent alarming parents and kids at parks, Erikson and other student researchers concealed the scary-looking air sampling machines in their cars, leaving only hoses sticking out of windows.
In response to the growing number of antibiotic resistant infections, the U.S. Center for Disease Control and Prevention (CDC) launched the Antimicrobial Stewardship Program, which encourages physicians to prescribe antibiotics only when needed. Meanwhile, in countries lacking sophisticated medical infrastructure, widespread use has become part of daily life—available over the counter, antibiotics take the place of good sanitation practices.
Overuse is also a problem in the livestock industry. In the U.S., it is estimated that 70 percent of antibiotics are used in meat production with virtually zero oversight, lead author Echeverria-Palencia said.
“Big Ag isn’t required to report what antibiotics they’re using and in what quantities. A few years ago, President Obama created a committee to assess antibiotic resistance, and he left out agriculture entirely. So, it’s this big powerhouse and nobody really touches it,” she said.
In China, antibiotic use on farms is even more intense. The antibiotic colistin—a last line of defense—has been liberally used in pig farming. It is no longer effective on animal infections, and resistance is suspected to be transitioning to people.
The ultimate result of antibiotic abuse could be a post-antibiotic world, and that has doctors like Romney Humphries, a UCLA clinical microbiologist, paying close attention. Humphries first encountered a patient with an antibiotic resistant superbug in July 2009.
“It was a really a big deal,” she said. “Now we probably have one a week, if not more. And it happened pretty quickly.”
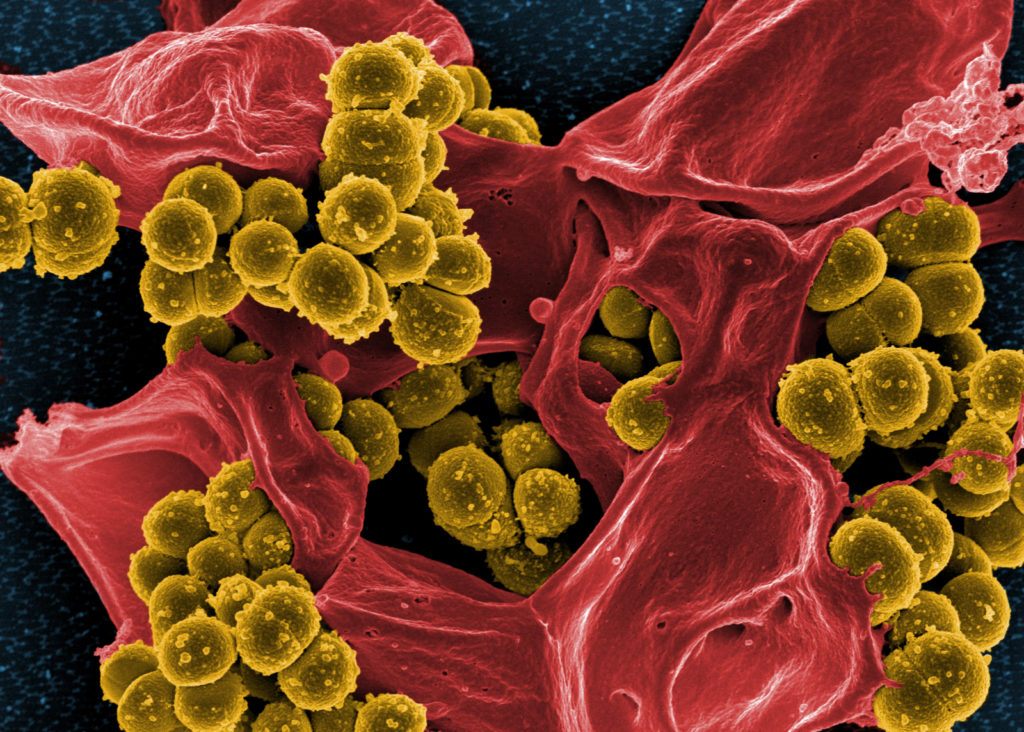
Top photo: A scan of methicillin-resistant Staphylococcus aureus. | Photo source: NIAID, Wikimedia Commons.
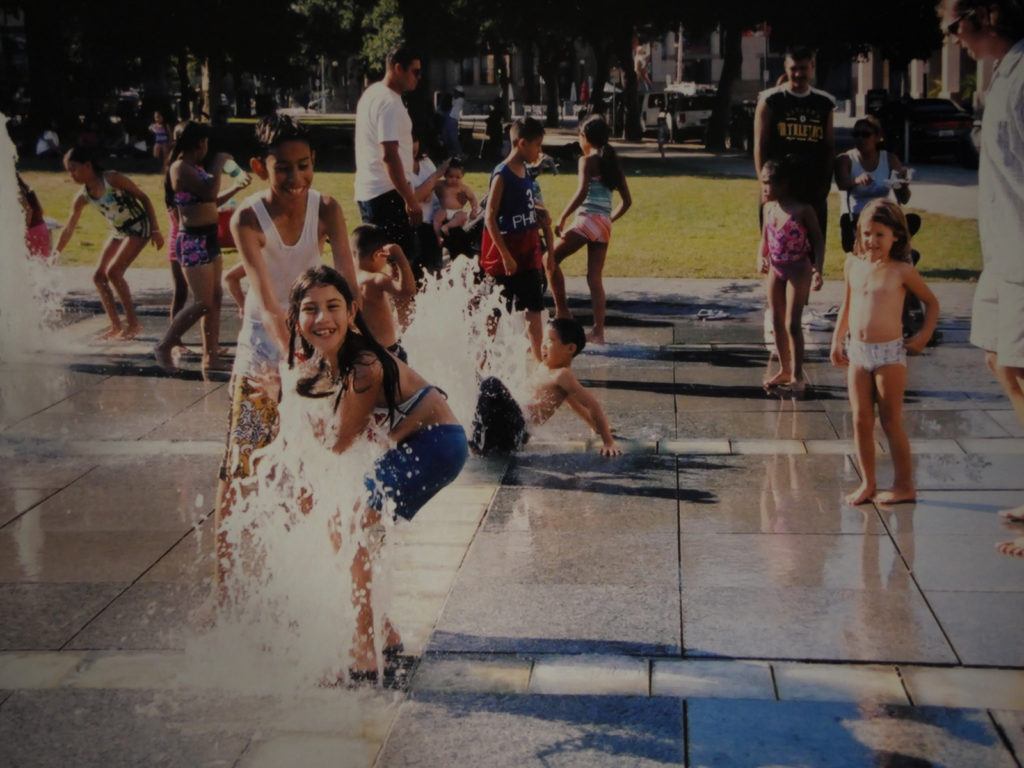
Second photo: Children playing in water fountains, California. | Photo credit: Belinda Waymouth




